I’m so grateful to Ida for sharing her story of hope and healing. Our paths crossed only recently but our healing journeys have run parallel for some time. She’s been a light and inspiration for me and I know others will benefit from her strength as I have.

Contender
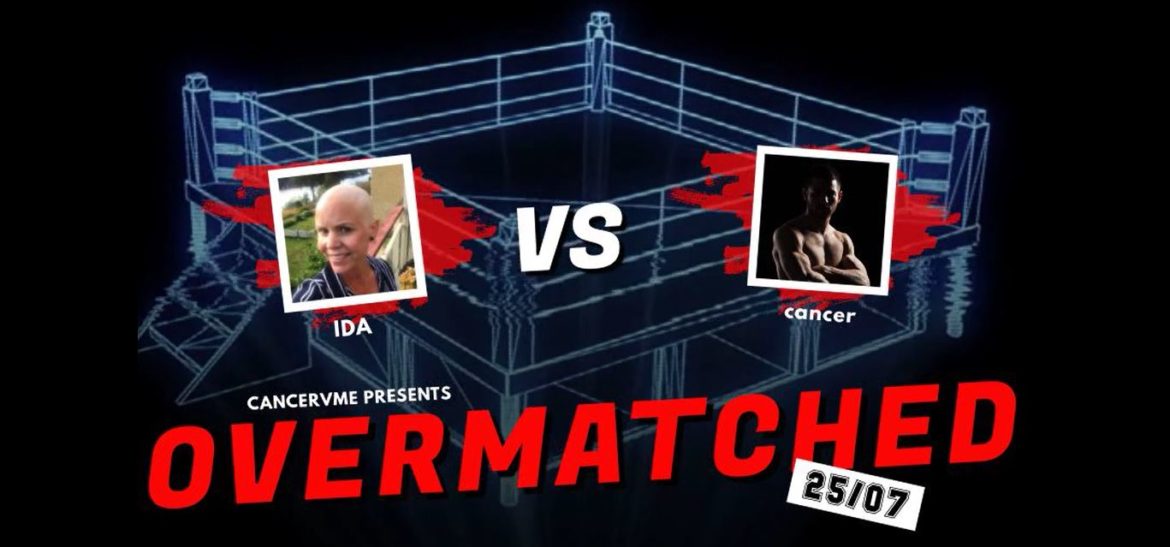
Ida Johnsson
Age at diagnosis: 36
Weaknesses: Stress
Strengths: Uncountable
Weapons: fasting, plant-based ketogenic diet, exercise, surgery, chemo, sufficient sleep
Follow her on instagram @plant_centric.keto for a rich source of healing inspiration
Opponent
Stage 4 Ovarian Cancer spread to peritoneal cavity, groin lymph nodes, spleen and liver
How were you originally diagnosed?
How I got my cancer diagnosis could be a story of its own, as I found lumps in my groins in December 2018 and got my stage lV ovarian (primary peritoneal) cancer diagnosis first in May 2019. This was a truly stressful period of going back and forth between hope and despair.
It took a while before primary care agreed to take biopsies of my lumps. However, when the results came back in March it stood clear that I not only had cancer, but, considering the cell types found in the biopsies, metastatic cancer.
Now things finally started to happen, and I was sent for a lot of examinations and testing. The CT-PET scan revealed that I had tumors in my peritoneal cavity, groin lymph nodes, spleen and liver. Stage lV cancer, regardless of the primary origin, this was per definition stage lV cancer. Also, I learned that the tumors in my liver were unresectable, making a complete debulking surgery, where all visible tumor mass is removed, impossible. Hence, they told me chemo was the only weapon against those tumors.
The primary origin of my cancer is believed to be an endometrial cyst close to one of my ovaries. The type is high-grade serous carcinoma, which is the most common and lethal type of ovarian cancer.

Were you given any specific prognosis or outlook?
My oncologist has been reluctant to give me a prognosis, as the outcome differs a lot between patients. Though, I have had a hard time not doing some research on my own.
According to the most recent local registry data, overall 5-year survival is 19% for stage lV ovarian cancer. That’s sad reading as it is, but my odds are even worse as a complete debulking surgery is the most important prognostic factor for long-term survival.
What conventional treatment have you received?
I have gone through initial surgery to remove all visible tumor mass in the peritoneal cavity. Though, the tumors in my liver, spleen and groin lymph nodes were left behind. Since then I have completed 7 rounds of chemo with the drug combination carboplatin and paclitaxel. In addition, I have also started maintenance treatment with Avastin, which is an anti-angiogenic therapy that interfere with the growth of new blood vessels.
I have just recently got my post-treatment imaging results and the only evidence of disease left is an area with minor irregularities on my right liver. From the picture it is impossible to say if that is a post therapeutic appearance or remaining tumor cells. To cite my oncologist, I am as close to be in full remission as you possibly can, without being declared as no evidence of disease. People around me say its great news that I am more or less disease free. Though, I see the area with irregularities on my liver as a reminder that the cancer may start to grow again and that I need to do what I possibly can to prevent that from happen, or at least slow down the growth.
Were there any physical symptoms before you were diagnosed that you only realize in retrospect were caused by cancer?
I didn’t experience any symptoms of the cancer itself either before or after I got my diagnosis. The only sign was the swollen groin lymph nodes, so without those metastases it would most likely have spread and grown considerably more before I got my diagnosis. To have no or minimal symptoms are common with ovarian and peritoneal cancers. That’s why most patients are diagnosed first in stage III or IV.
What was your lifestyle before diagnosis? Your diet?
The first potential harmful lifestyle factor that I had in my life before diagnosis was stress. Spring 2018, when I potentially started to get sick, given the growth and spread of my cancer, was probably the most stressful time in my life to date. At that time my oldest son was about 1 yr old and started daycare and I began to work again after my maternity leave. On top of working full time and taking care of our child after work, we had just bought a house that we were renovating, and I was pregnant with our second child. In retrospect, this is a period in life I probably should have worked part time or potentially not at all. Instead I worked way more than full time, as we were low on staff. To compensate for picking up my son early in the afternoons from daycare, I regularly did put in some extra hours in the evenings/nights.
This leads us to the second harmful factor I definitely had in my life, sleep deprivation. To go to bed too late and work in front of the computer the last thing you do before falling asleep are both bad habits. Besides that, I had a problem lying in the same position for too long being pregnant in the 3rd trimester and my sleep was also significantly impacted by lying next to a 1 yr old that preferably slept on me. Altogether, this made both my sleep quality and quantity worse than ever.
To have a ‘healthy diet’ and to exercise regularly are both lifestyle elements that I have considered important to have in my life. However, in busy periods with too much on the agenda I have often fallen out from the exercise routine. This is also true for the last year before I got my cancer diagnosis, with the only exception being stroller walks after giving birth to my second child. In hectic periods of life, I also tend to make poor food choices.
Spring 2018 was no exception, I ate too much, too frequently, and the wrong things. For me, a healthy diet has meant a low carb high fat diet, as that diet has hold me on a stable weight. However, in stressful periods of life, I have craved high carb foods and sugary snacks. So, while I sat in front of the computer I was snacking on sugary dried ginger, trying to convince myself it wasn’t too bad of a choice as ginger itself is considered good for you. After giving birth to my second son in June 2018, life became a bit less stressful and I slowly started to get back to my old ‘healthier’ eating habits with less carbs and started to lose the weight I put on during pregnancy. My healthy diet then consisted of lots of meat and full fat diary, with veggies as a condiment. The summer 2018 was the warmest in decades in Sweden, so all summer long we did put something on the grill for dinner and after putting the big kid to sleep we regularly enjoyed wine and cheese on the balcony. After summer and until I found the lumps in my groins, I continued on the low carb diet, but as I was breast feeding, I was quite liberal with the carbs and allowed myself to have some cheat days now and then.

What lifestyle changes have you made? What’s helped and what’s been discarded?
Like many cancer patients, I have asked my oncologist what I can do to aid my recovery and prevent relapses. She told me it isn’t much one can do and proposed that I should continue to live as I normally do. My own reflection on that response was that if I kept the same habits I had when I got sick, it probably would be a perfect environment for the cancer to continue to grow and spread. Therefore, I’m dedicated to doing my own research to see what the evidence base suggests and what lifestyles other cancer survivors have pursued.
I have only started my lifestyle changes and healing journey, but listed are some elements I believe are helpful:
Diet
I have switched to a ketogenic diet to restrict the tumors access to glucose, as ovarian bulk cancer commonly is sugar driven. To go keto was only a small step for me, as I have eaten low carb diet now and then during the last decade. The most notable change for me has been to stepwise reduce the amount of protein I eat overall, and meat and dairy in particular. The rationale for this change is to reduce inflammation linked to diary and animal protein and avoid excess protein from being converted to glucose. I still include animal products in my diet, but less of a quantity and products with higher quality, e.g. grass-feed beef and wild-caught fish. Nowadays, I view animal protein more as a condiment and focus on the most nutrient-dense items like liver, egg yolk and fatty fish.
By cutting back on animal products, I now have more room to eat yummy and nourishing plant-based food. What is great is that most food items claimed to have anti-cancer properties are veggies, berries, herbs and spices. So, things like cruciferous veggies, nutrient packed sprouts, polyphenol rich berries, and herbs and spices like oregano, cilantro, garlic, ginger and turmeric are regulars on the menu. Of course, taking the carb content into consideration. To boost the gut health and immune system, I also make sure to eat fermented food like sauerkraut, cocosghurt, and kimchi daily. Since I
made the above dietary changes, I feel a lot better and have more energy. Also, I have had stomach problems on and off for the last years, which now are totally gone.
What I also would like to mention is that before when I have eaten low carb, I have viewed that way of eating as a temporary diet for weight loss and allowed myself regular cheat days. Now I see healthy eating as a way of life, and I don’t foresee myself having a cheat day over the next years. Why I believe that to be true is because I really have transformed my habits and thereby what my body wants to be feed with. So now I fantasize about avocado salad, sautéed spinach with garlic and nut butter, instead of craving sugary snacks.

Rocking cancer’s face since 2018
@plant_centric.keto
Exercise
Studies have shown that regular exercise during chemo can reduce side effects such as fatigue and increase quality of life, both during as well as after treatment. Many of the studies have focused on resistance training, so with this in mind I bought my first gym card in probably over 5 years. I started lifting weights a few weeks before I started chemo with the aim to visit the gym at least twice a week. Now at the end of my chemo, I’m considerably stronger than before the treatment started and possibly stronger than I ever.
Initially after diagnosis I also started to run, which have been a go to training for me previously. Though, it didn’t feel totally right for me at this point in time. One reason was that I became worried that it would stress my body, as my body wouldn’t know if I run away from a tiger or just wanted to make my heart beat faster. For cardio training, I have therefore switched to power walking outdoor in nature instead. This is something that makes me relaxed, at the same time as I get some cardio benefits.
My plan is to continue to prioritize exercise also now when I’m done with chemo. The only struggle will be less available time now when I start to work again, as it then will be harder to put together the life puzzle with two small kids. Though, I’m determined to find a way to fit it in, as I truly believe that if I don’t take time doing things that make me feel well know, I may need to take time of being sick again later.
Fasting
I have fasted for 3-4 days during every cycle of chemo, as emerging evidence suggest that it can reduce side effects from chemo and boost treatment efficacy. So far, the number of studies is still few and small, but promising enough to make me a believer. I have only had minimal side effects from chemo and so far, no evidence of fatigue. Hopefully, there will be sufficient evidence in the near future so more patients can experience the benefits of fasting during chemo.
I also do daily intermittent fasting and aim on a 4-6 hours eating window, but between my rounds of chemo It has been more generous so I shouldn’t lose too much weight from the fasting. I view intermittent fasting as an add on to a ketogenic diet, as it helps lower blood sugar and increase ketone production. Also, evidence in breast cancer patients suggest that prolonged overnight fast reduce the recurrence risk and even risk of other cancers. What is great with intermittent fast is that I now feel less hungry and reduced need for snacking between meals, even if that still happens from time to time. Also, more time in the morning to focus on getting the kids ready before daycare has been a blessing.
I plan to continue with longer fasts now when I am done with chemo, but haven’t established a fixed routine yet. On a weekly basis I am now trying out how my body reacts to 40 hours fast on Mondays (Sunday dinner to Tuesday lunch) and 24 hours fast on Fridays (Thursday dinner to Friday dinner. Then I plan to do prolonged fasts 3-7 days at least every quarter. The aim with prolonged fasts will be to promote cell renewal and autophagy.
Stress reduction
While on sick leave during chemo, I’ve started with some anti-stress activities including yoga, mindfulness, taking morning walks in the forest by a nearby lake and sauna baths (so glad my husband insisted on us keeping ours when renovating the house). These are all activities that I will do what I can to continue have to some degree in my life also now when I am back at work again. To have a weekly scheduled yoga class and to do a few minutes mindfulness every evening before going to bed should be doable, but for sure I know that the morning walks and sauna baths will be fewer.
Therefore, I will see if I can find other tools to lower my cortisol levels, like possibly using calming breathing techniques while traveling on the subway to work. All suggestions are appreciated. But probably more important I will make sure to not be in the same stressful environment at work again. Start to say no when I have too much on my plate and never again work late at night to meet a deadline. This might be the hardest things for me to do as I have stressed and worked a lot during most of my grown-up life, but probably one of the most impactful.
Sleep
I really wish I could brag and say that I nowadays go to bed early and sleep 8 hours per night. However, sleep is an area that is really hard to optimize when you have two kids at 1.5 yr and 3 yrs. What I am doing, though, is to go to bed earlier than before, in order to get a few hours sleep before my youngest wakes up for the first time at night. Also, previously I had a hard time falling asleep, which isn’t the case anymore. For that I mainly thank my lower stress-levels and better practices around mobile phone use (not using it late at night, etc). Less food in the evenings supporting a healthy circadian rhythm and regular exercise may also play a big role.

@plant_centric.keto
What’s been the reaction of your healthcare providers?
My oncologist has not recommended any lifestyle changes but has mostly been supportive and accepted the choices I have made. She promotes being active during treatment, considering the research on benefits linked to exercise. However, when it comes to diet and fasting, she said that research is limited, but allowed me to do what I believe in and to eat what makes me feel good. On our post-chemo visit, my oncologist was surprised to see how well I am (no residual side effects) and admitted that my lifestyle choices and fasting may have played a significant role.
Prolonged fasting during chemo is the single element that I’ve needed to defend the most during my cancer journey. My nurse in the chemo ward said fasting during chemo was the stupidest thing she ever heard of in her 20 years of working. She refused to look at any research paper that I offered me to share with her and gave me a glass of sugary juice that she hoped I would drink.
Anything else you can think to share?
Many times, things such as a specific diet or supplement is marketed as a way to starve, kill or, cure cancer. Considering that cancer is a very complex and heterogeneous disease, I personally don’t believe that there exists one single miraculous thing you can do or eat to heal from cancer.
However, when used alongside conventional treatment and several elements in combination, I truly believe that lifestyle factors can be a powerful tool to better your odds and increase quality of life for cancer patients. Even if the lifestyle changes I’ve made only delays progression with a few extra months, I would see that extra time to enjoy life together with family and friends as extremely valuable. In particular, if I can feel as healthy and good as I am doing right now.
Also, I work within pharma, so if there’s something I know, it is to never underestimate the power of the placebo effect. To me it means that I relay on my gut feeling and that the lifestyle elements I really believe in probably will be the most successful.